Reading: Elements of Electronic Health Records (EHR)
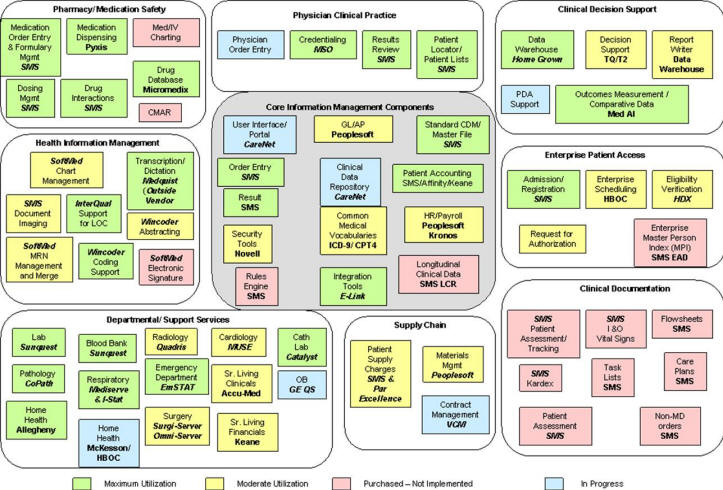
Electronic health records are used in hospitals, physician offices, integrated health maintenance organizations, and other generators and users of health information. Consumers may also maintain their own personal electronic health record. The uses of electronic health records in the health care industry is growing. Electronic Health Record may be defined as a database and associated application software that a provider maintains regarding patient's wellness and encounters with various health care services. A comprehensive electronic health record has a large number of subsystems. Almost no one needs all the subsystems. What a physician's office needs and what an acute hospital need maybe quite different. Here are a set of basic, standard or add-on subsystems. The basic sub system of EHR may include Accounts Receivable, Consolidated Mail, Outpatient Pharmacy, Controlled Substances, Current Procedural Terminology (CPT), Diagnostic Related Group (DRG), Grouper Drug Accountability/Inventory, Interface, Duplicate Record Merge: Patient Merge, Event Capture, Medications, Inpatient Medications - Intravenous Inpatient Medications - Unit Dose, Integrated Billing, Laboratory, Laboratory Electronic Data Interchange, Lexicon Utility, Master Patient Index, Master Patient Index/Patient Demographics, National Drug File, Outpatient Pharmacy, Patient Information Management Systems (Admission, Discharge, Transfer, Registration), Pharmacy Benefits Management, Pharmacy Data Management, Radiology/Nuclear Medicine, and Scheduling. The standard EHR may include Adverse Reaction Tracking, Authorization/Subscription Utility, Automated Information Collection System (AICS), Automated Medical information Exchange (AMIE), Automatic Replenishment/Ward Stock, Clinical Reminders, Consults/Request Tracking, CPRS, Dietetics, Generic Code Sheet, Health Summary, Integrated Funds Distribution, Control Point Activity, Accounting and Procurement (IFCAP), Patient Care Encounter, Problem List, Text Integration, Utilities, and Vitals/Measurements. Add-ons to Electronic Health Record may include Equipment/Turn-In, Request Fee Basis, Hepatitis C Extract, Home Based Primary Care, Immunology Case Registry, Incident Reporting, Intake and Output, Library, Medicine Clinical Services, Mental Health, Minimal Patient Dataset, Network Health Exchange, Nursing, Occurrence Screen, Oncology, Patient Identification Card, Personnel and Accounting Integrated Data, Pharmacy Prescription Practices, Police and Security, Primary Care Management Module, Prosthetics, Quality: Audiology And Speech Analysis And Reporting, Record Tracking, Resident Assessment Instrument/Minimum Data Set, Risk Assessment (Surgery), Social Work, Spinal Cord Dysfunction, Surgery, Survey Generator, Visual Impairment Service Team, Voluntary Timekeeping, and Women's Health. As you can see, it is difficult to define what is an electronic health record. The definition changes often and components included or excluded vary depending on various vendors. Claudine Beron implemented VistA at one organization. Several components of VistA were implemented, some were not. Figure 1 allows one to glance at the various sub-systems implemented and how they related to each other. Because electronic health records are complex and large, at any one point, several components of the system may be in the process of changing. In Figure 1, systems implemented and in heavy use, systems implemented and in moderate use, system purchased but not implemented and systems planned but not purchased are shown in different colors, .
Figure 1: Claudine Baron's description of Various Components of Electronic Health Record implemented This page was organized by
Farrokh Alemi, Ph.D. Last date of revisions was on
|