
Online Health Records
By Bruce Slater, MD, MPH
University of Wisconsin School of Medicine and Public Health
This presentation will compare the history of paper and electronic
patient records, describe the major elements of the electronic health
record and explain how electronic health records are different to the
paper patient chart
Healthcare lags behind many aspects of our lives in automated
information use. Although computers are used in financial transactions
and clinicians use the web for medical and non-medical information
searching, only a minority of physicians use it for storing records.
Electronic Patient Record or EPR and the Electronic Medical Record or
EMR are two names for a similar concept. Physicians typically talk about
Electronic Medical Records while nurses, public health and more
holistically oriented commentators use the Electronic Patient Record
description.
The Computer-based Patient Record, CbPR or CPR for short is the name
chosen by the Institute of Medicine in it’s landmark report in 1991
promoting the use of computer systems in Health Care. In addition to
medical and non-medical health information, the CPRS incorporates and
enables communication, education, analysis and quality control into a
single comprehensive birth to death nationwide system. Ultimately we
have backed off a vision of a monolithic national system in favor of
many systems hosted by healthcare organizations that are able to
communicate via national standards and information interchange networks.
The missing aspect of patient input is included in the most recent
moniker Electronic Health Record or EHR.
After the rise of the stand-alone personal computer we re-discovered
the power of linking computers together. Instead of linking dumb
terminals to mainframes, we divided the power of the main frame into a
Client-Server pair connected over a Local Area Network (LAN). The client
handles the presentation of data to the user and the Server stores files
and does database lookups and serves the data or results back to the
client for action.
In the ASP or Application Service Provider model, the internet has made
it possible to move even more of the processing to a remote site.
Intended for small scale operations that cannot afford a full
client-server EHR an ASP company will purchase the EHR license, the
hardware and the expertise to it and then offer “slices” of the full
functionality to individual practices. Subscribers do not have the large
up-front costs of the full software license, expensive fault-tolerant
servers and expertise of the full support model. ASP companies can fully
exploit the robust applications by selling 100% of the EHR capacity to
many small users. Properly done the ASP model can be a win for both
subscribers and service providers.
When humans discovered that certain of their group had special powers
to heal the sick and comfort the dying they designated them shaman. All
cultures gave their shaman special dispensation to access intimate
aspects of the human body and use potentially dangerous procedures and
potentially poisonous treatments. Shaman trained apprentices by the oral
tradition to follow their practices. When writing became common place it
still took centuries until written records were kept in hospitals. It
seems we have always been behind the technological time. These hospital
records were kept in ward notebooks and they documented the condition of
patients, results of tests and opinions of consultants for the current
episode of care. For the patients in an early 1800’s hospital, a
physician could look back to previous ward book entries, but records
were not generally organized by individual patients. Florence
Nightingale is credited with keeping patient-oriented health records in
the Crimean War in the 1850’s. As healthcare became more technical and
involved many different specific tests and treatments in the 1950’s,
practitioners began to sort the results by their source. So-called
source oriented documentation prevailed for decades in hospitals and
outpatient records. Dr. Larry Weed promoted the concept of medical
records that guide and teach in what he called problem oriented medical
records. He organized his in- and outpatient notes by the (S) subjective
or historical aspect; the (O) objective observations that were
independent of what the patient said; the (A) assessments or assertions
of diagnoses or problems and the (P) plan both therapeutic and
diagnostic. Using the mnemonic of S.O.A.P. all students have been taught
for the last 20 years to keep records in this problem-oriented way.
Creating this kind of record while listening and examining the patient
enables providers to have a running list of issues that must be
addressed in the visit. Although Dr. Weed anticipated implementing
problem oriented medical record in a computer, ironically the SOAP notes
inspired by him have increased the volume of paper records as well as
inspiring electronic versions. As the paper record becomes more
voluminous and central to patient care the lost and incomplete paper
chart has become a chronic challenge to every health care delivery
system.
Dr. Weed always intended his Problem Oriented Medical Record to be
based in a computer. The linkages between the problem list and
individual problem based progress notes can only be done virtually.
Expecting providers to manually track problem numbers between problem
lists and progress notes has led to incomplete records in almost every
instance. To make this possible Weed created the PRoblem Oriented
Medical Information System or PROMIS. Unfortunately the promise of
PROMIS was not realized. Success depended on a very strict use of rigid
text boxes and required fields. Providers, on the other hand, tend to
talk informally with patients and ideally have patient-centered not just
problem oriented interviews. The rigidity of PROMIS was not well
accepted by practicing doctors and the software never caught on. Another
effort shortly after in the early 70’s was made at the Massachusetts
General Hospital. It was intimately related to the development of MUMPS
(MGH Utility Multi-Purpose System) programming language. Many
applications were developed in this language. The COmputer-STored
Ambulatory Record or COSTAR was one of them. This was very strongly
problem-oriented, used a data dictionary to codify the data that it
contained and had a very sophisticated query generating system to
extract data from the database. In addition, it was public domain.
Unfortunately, it’s strong points also became it’s downfall. Because it
was public domain, no company successfully standardized and carried all
of the variations that became available, into the future. For many years
it was the system of choice for public institutions without a budget to
support proprietary systems. Many COSTAR systems, especially at MGH and
Nebraska have prospered and assisted in patient care for over 20 years.
MUMPS, however, lends itself to spaghetti (or excessively branching)
code which is essentially impossible to maintain by a team of
programmers. As programming languages progressed to 3rd and 4th
generation and true object-oriented approaches, MUMPS usage for new
projects ended. Therefore no new MUMPS programmers are being tutored and
COSTAR is fading after a long and illustrious career.
Practice Partner started life as a DOS-based EMR with a proprietary
database format. It has progressed to a MS Windows interface, and is
available with an Oracle database. It is sold through a national network
and has been around for many years. It uses the typical “tab” metaphor
to mirror the look and feel of a paper chart. This is the same metaphor
that has been used in many EMRs since the windows interface has become
available. Practice Partner has been around long enough for interfaces
to have been built to major national labs. The company leverages the
advantages of a large population of users on the same system to
aggregate clinical data and form a research network. They also offer
benchmarking services between and among the large population of users.
They have developed web access to their product, a patient portal and
have offered it as an ASP solution. Medicalogic is another system
founded and programmed by a physician and born as a DOS program. It is
now available as a client server Oracle based system. The Windows
version was called Logician and has a strong user group and shares
templates among users. It has been purchased by McKesson and folded into
their Centricity line of software. EPIC or EPICare is written in a
language similar to MUMPS and has a proprietary database. For small
practices it is very expensive. For very large practices, it can be
economical and has had its biggest success in massive networks like
Kaiser Permanente. It does have a windows interface and web versions. It
seems the common denominator for many existing systems and some new
systems is a web orientation.
“The Chart” is what providers ask for first. In the outpatient
setting, it has the lifetime history of the patient, unless you only
have the 5th of 5 volumes. If the file clerk doesn’t check and brings
you the 4th of 5 volumes, it doesn’t help much at all. In the inpatient
setting, there is no lifetime history. To the “modern hospital”, as in
the first hospitals, only the current episode of care has any meaning.
Because hospitals generate massive amounts of paper, it would be
impractical to present the user with a lifetime record. They couldn’t
likely carry it around anyway. As any paper folder has a tendency to
tear and degenerate, a trade off in quality of materials has too be
made. Expensive folders last longer, but cost more. The filing system
used has to be chosen carefully. Most small operations file by last
name. This creates a problem when people marry or otherwise change
names. It requires all of the diverse cultures to adopt the
Judeo-Christian format of names which can cause confusion. Most large
systems require patients to have a medical record number (MRN). Some
hospitals call it a “history number”. This frees the system from
reliance on names. Unfortunately it creates its own conundrums.
Duplicate MRNs can represent up to 20% of charts. Information filed
under a duplicate is unavailable to the treating provider. To prevent
the size of the medical records department from increasing and taking
over the whole care setting, some thinning must be done. Charts of
patients not seen in a certain time, usually 3-5 years are boxed and
removed to an archive location where square footage is not as expensive.
Unfortunately if the patient returns from a long absence and needs care,
there will be a delay in retrieving the previous information. As you can
imagine the archiving process offers multiple opportunities for losing
information. A careful record of which charts go where and when was the
last visit was must be kept. Among active records, tracking exactly
where a chart is constitutes a large part of a medical record
technician’s time. If a chart is pulled from the shelf for a phone call
and then returned to the file room, it must be retrieved for a scheduled
visit. If the scheduled visit is in urgent care the same day, it
requires an extraordinary system to get it to where the patient and
provider are meeting. Bar codes on each chart can help, but add a layer
of work and expense in keeping track of them. The physical folder
becomes a marker for itself. The only way to know if you have the
information is to hold it in your hand. Of course, the physical folder
can only be in one place at one time. Auditing a chart takes it out of
circulation. When a provider holds a chart as a reminder to follow-up on
a patient, that makes the chart unavailable for other caregivers. For
the very sick patient, in the hospital setting it is very common to have
3 or 4 individuals with an interest or need to have the chart at the
same time.
Realizing that paper charts were a poor basis for a sophisticated
information system, medical records professionals tried to improve them
by adding additional labels and flags. A physical patient folder is not
intrinsically identified until a physical label with either a name or
number is placed on it. A sticker is placed when a file is accessed for
the first time in a given year. This is used to indicate when the folder
should be archived. Allergy warnings are placed on the outside of the
folder, but may not be kept up to date or reviewed by all providers and
therefore are ineffective in their purpose. Sometimes birth dates are
put on folders. Some departments place insurance information on folders.
All of these are symptoms of an inadequate information system starting
with the paper folder. Within the paper record there is typically an
insurance form filled out with insurance account numbers, next of kin,
sponsor information and in many practices there is an initial history
form. All these forms contain information that changes. They contain a
mixture of administrative and clinical information. The chart is
typically the purview of clinical professionals and doesn’t routinely
get routed to administrative personnel to keep the information up to
date. The clinical information recorded at intake is a snapshot at best
and doesn’t fit into the usual workflow of the provider. One of the
quality markers looked for in audits of patient charts is a problem list
that is up to date. The paper problem list is either ignored or
inadequate. For simple problems providers don’t feel it necessary to put
everything on the list. For complex patients with multiple interacting
problems, there is no good way to represent the relationships between
the problems. As an additional disincentive, in a capitated environment
the complex patients are reimbursed at the same rate as simple patients
and therefore there is no time to do the additional paper work of
keeping the problem, medication and allergy lists up to date. Looking
for a progress note or lab result related to a problem list item is all
but impossible in most paper based systems.
Within paper records whether they are true source oriented, which is
rare today, or nominally “problem oriented”, there are dividers in the
chart which indicate where the documents come from. In essence all paper
charts have to be source oriented.
Progress notes, lab results, radiology results, consultant notes are
all kept in separate divided areas of the chart. Providers frequently
like to compare lab results over time. If lab results were filed with
the progress notes that generated them, that would not be possible. Also
lab results related to multiple problems are ordered and reported
together, so it is essentially impossible to have true problem oriented
paper records. In order for billing to be supported, each progress note
and consultation report must include much redundant information. This
generates massive amounts of text for documentation purposes only which
does not contribute to a provider’s understanding of the patient’s
problems. While searching for relevant information, this boilerplate
text just gets in the way.
Another bad habit made necessary by paper records is the recording of
clinical information on lab and x-ray result documents. Ideally every
provider would request the chart to be pulled from the record room to
document the results of every lab and x-ray. In this way the notes
relevant to the care of the patient could be appended to the progress
note that generated the test or x-ray order. When subsequent providers
or students review the chart, they can follow the notes that the
provider makes to guide their understanding of the provider’s thinking
process and teach students the “why” of what they did. This is in the
best tradition of Dr. Weed’s vision of medical records that guide and
teach. In the real world, providers look at a result and try to remember
the patient, make a note on the report itself about what is to be done,
or document that they discussed the finding with the patient all without
benefit of the rest of the chart. Pulling the chart each time would
double or triple the work that the already stretched medical records
departments do. If the provider elects to keep the chart until the
results come back, another inadequate situation develops. If the patient
delays getting the test done, the chart could sit for a long period of
time and be unavailable for patient care or audit or administrative
functions. The medical records personnel are judged on what percentage
of charts they can deliver and these sequestered records are not
available. Chart sweeps to open doctors’ offices and pick up piles of
charts are sometimes done which completely destroys the reminder
function of the paper record. Many providers have a “shadow record”
where they keep reminder information which must be duplicated to the
paper record at some point. There is no theoretical scenario in which
paper records could be made ideal even with massive personnel support.
Although electronic systems that are truly “paperless” are few, as
more of the patient record function is moved to networked computers, it
becomes more of a virtual record. Most practices that use electronic
records still print and file documents in a traditional paper chart to
satisfy legal requirements for pen and ink signatures. Legislation that
has legalized electronic signatures in some areas has helped move
electronic records forward. A virtual record does not have a physical
location. It is pure information. You can not point to a standalone
computer or even a network server as the location of the information. In
some systems part of the information is embedded in the client software
or browser and other parts in the server database. Replication of
databases and backups create equivalent copies in multiple places.
In a virtual record there is no limit to the number and kinds of
flags and labels that can be applied to a patient’s record. The physical
paper file no longer has to be the marker. Multiple volumes are not an
issue. You no longer have to decide on a single filing system. All
records are filed by a primary key which by definition has no relation
to anything specific about the patient. Charts are not filed by Social
Security Numbers, history numbers, MRN, birthdays, phone numbers or
names. Because of this ANY of the foregoing can be used to locate
records, which should be purpose of “filing” records. When you have a
virtual record the concept of an enterprise master patient index (EMPI)
starts to make sense. The EMPI keeps track of each specific system’s
identifying information for the entity known as the person. Creating
duplicate records for the same patient is much less likely when all the
details are brought to the attention of the registration clerk.
Instead of duplicating computer based demographic and insurance
information into paper forms in a paper chart, the virtual record simply
links to the actual information in a table. This is where the owner of
the information will be keeping it up to date. When all information
users reference a single information source, less mistakes and re-dos
are necessary resulting in a higher quality, more efficient service.
A problem oriented patient record starts to make sense if it is
electronic. You can use the problem list as an index of the medical
record. All references to a problem can be accessed by linking from the
problem list. The medication list is always up to date because that is
how medications are prescribed and refilled. The allergy checking
function becomes a prominent part of practice by fading to the
background, but becomes 100% effective.
Instead of depending on a few preset dividers to organize the
information in the chart, a provider can choose any number of ways or
“views” for his or her charts or for a particular chart. “Thinning” a
chart is when a medical records professional tries to imagine what a
provider no longer wants to see and takes it out of the the paper chart.
With a virtual record each provider can create any number of ad-hoc
thinned charts.
The progress note function can be divided into various purposes. At
some point, payers will realize Evaluation and Management (E&M) coding
is passé and adds no value to the interaction. Until then providers can
still instruct the EHR to create “progress notes” to satisfy whatever
coding level they believe is appropriate for a visit. If on the other
hand, the provider wants to view the data in a more efficient manner a
view can be constructed at any time since the data is coded and remains
unchanged in the underlying database.
Instead of always reading the transcribed reports of radiologists, if
the institution has an electronic image archive, the primary care or
other specialist can look at the actual image on the screen to explain
to the patient or double check for themselves.
One of the most powerful reasons to evolve to the electronic record
is security. The roof leak or flood scenario could put a paper-based
organization out of business. Paper records can be physically stolen and
there is no backup available. Paper records can be photocopied and there
is no way to detect the act. Anyone with access to the file room
technically has access to stealing, altering or copying any record from
the shelves. Electronic records can never be stolen or damaged if
backups are properly done. Everyone who accesses a record for whatever
reason can be audited for review by a appropriate security official or
by the patient themselves in some systems. No copies or alterations are
possible without leaving an audit trail. We can give certain people full
access to a particular record for audit or other reasons and they do not
inherit access to any other record. Currently it is against any medical
records organization rules to physically take records out of the
building. There are many good reasons to have this rule. It is routinely
broken in some organizations by well-meaning providers who can’t get all
the work done during the day and need to finish documenting at home.
With an electronic system, it is unnecessary. A particular chart can be
securely viewed anywhere in the world with proper security precautions
that have already been established and tested in the banking world. In
the same vein a chart can go with the patient to the cardiologist and be
back for the primary care visit even if the appointments are minutes
apart because the chart never actually goes anywhere. Paradoxically, the
chart can go more places because it doesn’t actually go anyplace!
One of the markers of a high quality product is reduced variability
in the final product or service. With paper records it is so inefficient
to tell exactly what kind of care is going on that only with a huge
budget is serious quality control possible. By careful design of
templates and data dictionary and automatic 100% auditing of important
aspects of care, the virtual record makes consistency and high quality
attainable goals.
Reminders in a paper system are of two kinds. The chart surrogate is
the most common. Keeping the chart as a marker for a sick patient or an
important result does work, but the chart is unavailable for other
unrelated care in other locations. The other reminder occurs when
providers create a “shadow chart” by keeping a separate note book of
patient names, medical record numbers, multiple contact numbers, an
abbreviated problem list and the actual reminder. Then they can manually
review the list at intervals to see whose results has not come back.
Even so, chart pulls are required to check on details and document
results taken over the phone. The frequent, tragic and needless failure
to diagnose cancer and other serious illness because of failure of the
reminder function should embolden providers to try anything else because
of the manifest failure of paper systems or at least the tremendous
additional labor involved if they are properly done.
From time to time in looking at paper charts providers will come
across an article photocopied and stapled or bound into the record. This
may have been from the patient or a student and would likely have some
tangential relevance to their conditions. Instead of being the
exception, an intelligent virtual record could have routine protocols,
care paths, guidelines and evidence based advice just a click away.
Link-outs are possible in a virtual record connected to the Internet.
Even if the record is stored on a single computer and inaccessible from
the internet, a link to a library of full-text references could add
measurably to the care of the patient.
Reminders, embedded Intelligence and Link-outs are a feature of
Electronic Health Records called Clinical Decision Support which is not
available in paper records. Features such as evidence based order sets,
evidence based templates for progress notes are another form of clinical
decision support not as easily provided in the paper record.
The busy provider rarely has time to notice the random photocopied
article in the occasional chart. To enhance a patient oriented
education, they could jot down the reference and look up and study the
article. But the reference could be tangential or exceptional and not
helpful for most other patients. What if the provider could leave a
bookmark in the chart of a patient - not visible to other providers or
auditors or to the patient, but kept in a special place that the
provider could reference from home or elsewhere during a continuing
education activity? What if providers could actually list their
information needs without making that knowledge known to anyone else?
What if they could audit themselves and design an education program
specifically for their weaknesses and in the light of their learning
style and strengths in other areas? Or better yet what if their
information needs were anonymously feed to specialist in the appropriate
area to have a suggested program designed for them and feed back
anonymously? Why not give them CME credit for actually looking up and
learning information in the course of their daily practice? The current
answer to these questions is that it is impractical or impossible. With
a virtual record it becomes possibly to seamlessly transition from
patient care to professional education.
Many electronic systems currently have extensive patient education
modules. It is a small step to create mass customization for each
patient’s problem list.
Extending the ability for patents to read and contribute to their
record is available in many EHR systems. When patients are finally
incorporated into their care the concept of problem orientation will be
the only reasonable way for them to look at the chart. Patients are
expert at what bothers them, but clueless about ICD9 and CPT codes that
payers require.
The ability of a system to be organized truly in a problem oriented
way will separate the pack of contending vendors. The data will be
stored in a fully coded technically correct manner, but the various
views will be enabled depending on the needs of the user.
It is very expensive to audit paper records. If you can’t read a
contributor’s handwriting it is impossible to audit the care they are
giving, appropriateness of their reimbursement coding or in some cases
even know who they are! Electronic records can audit themselves. Audit
could become enmeshed in the continuing education that a provider
designs for themselves. Some of the reasons for auditing will disappear.
Use of appropriate E&M templates will ensure that appropriate codes are
being submitted as a matter of course. In the future, as the more
complicated systems come into use, the knowledge of coding will become
so arcane that no human could do it in real-time anyway. No “education”
will be needed because the need for the skill will go away!
Demand management is the managing of demand for health care. As any
provider will tell you, if you don’t have the diagnosis after taking a
careful history only a few strikingly unexpected physical exam findings
will help. The physical exam only confirms your suspicions in most
cases. If history taking could be automated and monitored over the web
in real-time by nurses backed up by physicians, the demand for actual
face-to-face appointments would decrease. Much of health care could be
accomplished over the web with brief confirmatory visits in some cases.
When actual visits or phone conversations are deemed necessary,
access management comes into play. Locating resources to match patients’
needs is best done by cell phones augmented by portable networked
information appliances. In the current model physicians are called and
have to be brought up to date or up to the minute on a patient’s status.
If the physician had a summary of the patient’s status they can
contribute immediately or preemptively to the care of the patient and
avoid the need for an actual phone conversation and the “bringing up to
date” function. Virtual records like EHRs can take health care to the
next level of value for patients and providers.
The thrust of electronic commerce or e-commerce is to become
intertwined in the daily routine of users. Whether it is banking
services expanding into full financial services or bookstores selling
items with no relation to books, e-commerce seeks to enmesh itself, add
value and become transparent to the user.
E-commerce has to first create the need for itself. It must do
something so much better than the bricks and mortar alternative that
people chose to migrate their activities to the virtual sector and
abandon their old ways. In all sectors this is difficult. In the health
sector we have a few things pushing us to the electronic realm. Bricks
and mortar and face-to-face are expensive compared with web access
anytime and anyplace. If we design systems that look and feel like the
providers workspace and create value for patients to exploit, the public
will assign electronic healthcare “need” status. It may be by
financially competing so intensely with bricks and mortar that a
face-to-face encounter will become an extraordinary and expensive event.
People have shown they must have value to change established patterns.
An inferior service at a lower cost will not likely prevail, especially
in a robust economy where people can well afford the current cost of
face-to-face care. A service that cost the same or less out of pocket,
but is easier to use, quicker to get to, automatically follows up on
treatment plans, educates you and connects you more closely to your
provider will drive traditional healthcare services out of the market.
It is likely that a bricks and clicks strategy or a symbiosis of
existing physical entities will prevail. In that model, most of the care
could occur virtually using EHRs. When a physical visit is needed, the
established physical entities like clinics and hospitals will be needed.
If a large percentage of care occurs without a visit or phone call by
interactive history taking guided by a mid-level provider or nurse, a
practice can take more capitated lives. They will still need to see
patients but they become more efficient by avoiding unnecessary visits.
When patients use the service as a matter of course, provider
organizations can extend into health related areas. Discounted exercise
equipment linked to the web for feedback into your personal exercise
program, grocery buying with reminders for healthy foods and feedback
about total calories, disease specific extensions of care beyond
traditional medical care into life enhancements chosen by the provider
are all made possible by a virtual practice. Providers still have the
ethical responsibility to put their patients’ welfare above profit.
Endorsements and web-site links have to be chosen with this in mind, as
always. It may be controversial, but this evolution can be done in a way
to preserve the best of the healer-patient relationship. Ultimately it
will start when we give ourselves permission to re-define healthcare in
a broader way and it will thrive when we immerse our patients in mass
customized health promotion messages.
Any EHR must be built on a repository of clinical data. Some have
designed the repository into the EHR itself. EpicCare is an example of
that kind. Other EHRs keep some of the data themselves, such as the
clinical notes the system generates itself, but links to a repository of
lab and other results. A Clinical Data Repository (CDR) is characterized
by having patient identified real-time clinical operations data in a
normalized form that is coded with a data dictionary. It is optimized
for individual patient centered queries and not research queries across
multiple patients, although theoretically those queries could be run.
The CDR is the source of results for providers seeing patients. The lab
and imaging results go directly into the CDR for immediate availability
for in and out patient care. The portion of the CDR for clinical images
is called a Picture Archiving and Communicating System or PACS.
Interfaces are built, usually using the HL-7 or ASTM standards to
existing legacy and reference lab systems. Different codes from feeder
systems are standardized into a common lexicon so that results can be
compared between systems if a patient’s insurance (and therefore
reference labs) changes. Some pure CDRs have gone into the EHR market by
improving their user interface and adding EHR-like functionality and
decision support tools. Ultimately it may be hard to decide between the
two kinds of systems. In a large enterprise a better choice will usually
be a CDR due to the need for robust large scale data manipulation. In a
small enterprise a pure EHR will frequently be the best choice for
economic reasons. The CDR can contain outcome measures and is the
enabling technology for population based care and research. In a pinch,
limited research queries can be run during idle time in the evening and
weekends on a pure CDR database without creating a research data
warehouse.
Practice partner and Logician are two products that have paralleled
each other’s development with Practice partner targeting small to mid
sized practices and Logician targeting mid to large organizations. Now
that both have developed web based products or delivery mechanisms, they
compete in the same niche. Patient profile is an system created by an
attending physician and a resident programmer in Microsoft access for
local use in a clinic. It is shown to demonstrate some generic qualities
of EHRs.
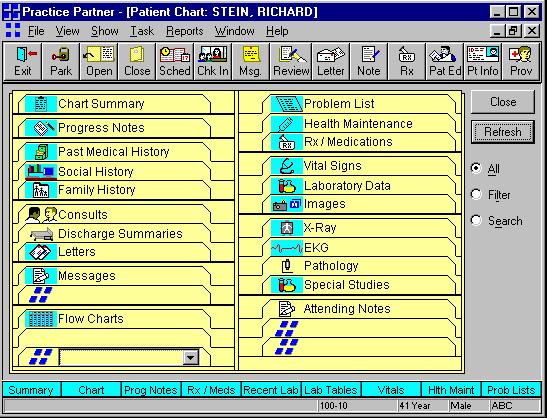
Figure 1: Example of Use of Tabs in Practice
Partner
The tab metaphor is a very powerful one for designers of EHRs. The
security of a paper metaphor is too strong to be resisted, so many EHRs
that have progressed passed the cascading menus of DOS programs use this
appearance. With most programs, there is more than one way to accomplish
a task. IN Practice Partner (Figure 1) ,the large buttons on top expose
the same functionality as the tabs in the foreground. The chart summary
is top left followed by progress notes since they have the summary of
most recent events. The main past history which changes only slowly is
Past/Social/Family history. The next section is consults, discharge
summaries and letters followed by messages and flowcharts. The problem
list occupies the predominant position on the right side of the screen.
The health maintenance area is conveniently located below problems and
above the Rx pad. For detailed data the vital signs, lab data and images
are next followed by x-ray, ekg, pathology and special studies. The
design is very flexible and most tabs can be rearranged or omitted.
Logician Internet uses the typical web page format with hierarchical
information on the left and details in the right frame (see Figure 2).
Information starts from most general at the top left:
- Chart Room
- Desktop
- Demographics
- Chart Summary
- Previous Notes
- Chart Notes
The Logician Internet web technology is improved by being implemented
in Java on the local machine to avoid variable network delays in screen
refreshes and enables a complex and detailed program. This creates the
need to synchronize the local database with the reference database and
also between different users of the chart.
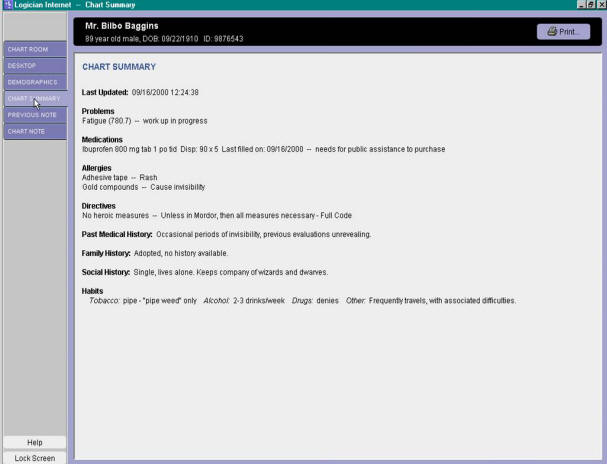
Figure 2: Display of Information in Logician
Electronic Health Record
Profile has functionality for prescription writing which goes beyond
it’s CDR function (See Figure 3). In this screen you can see behind the
pop-up to see lists of Allergies, Active Medication and Discontinued
Medications all together for easy reference. In the background are the
other typical tabs of the EHR chart sections. The pop-up gives the
impression of a written Rx which is called an affordance. That is it
affords the opportunity to enter prescription information. The central
drop down has a list of all medication available. The list is available
on the web and can be updated on a weekly basis. Below the drop down is
the free text Sig: area followed by the amount dispensed, the type of
preparation and number of refills, the start date, the prescribing
doctor, some free text notes and a link to a problem from the problem
list. On the right you notice the formulary area which would indicate
the formulary status and alternate suggested drugs. By having a list of
medications a provider can check off which ones to refill and make a
repetitive task easier.
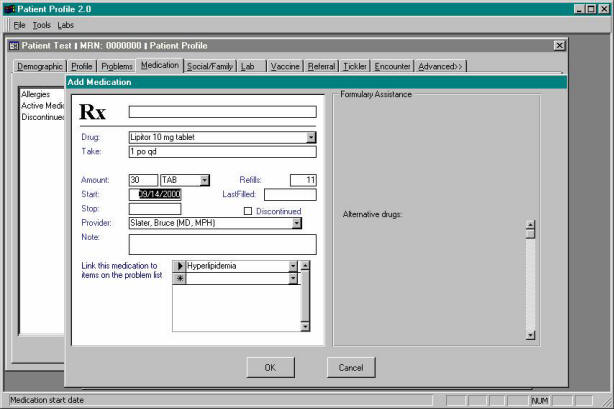
Figure 3: Functionality for Prescription Writing
in Profile Electronic Health Record
The Regional Health Information Organizations are
organized to facilitate exchange of information among health care
providers. George Mason University is proposing to organize one
such organization to serve providers of care in wider Washington DC
metropolitan area. The goal will be to allow designated providers
access to the patient’s complete record independent of where the patient
has received services. The organization will enable large and small
health care providers to effectively communicate to each other about the
care of their common patient.
A test ordered by the primary care physician will be
readily available to the specialist and vice versa.
In addition to improving patient safety and
quality of care, the integrated data is expected to reduce overall cost
of care, enhance health services research, enable detection of public
health outbreaks, and improve patient’s access to health information.
Principles of Operation
The Regional Health Information Organization (RHIO)
will be based on the following operation principles:
1.
Voluntary. Health care organizations voluntarily
choose to participate in RHIO.
2.
Public notification. Participating health care
providers will prominently display a sign informing their patients of
the organization’s participation in RHIO.
3.
No centralized database. No data is maintained by
RHIO. The organization maintains communication protocols and maps of
data structures, which will enable transfer of data from one
participating organization to another. RHIO does not require a uniform
data structure among all participating organizations.
4.
On demand transfer of data. At point of care and on
demand, RHIO will enable a provider of care who has client’s permission
to gain access to all data on the client in participating
organizations. Each participating organization will process the request
for transfer of the data on demand.
5.
Algorithm based record identifier. RHIO will not use
any unique identifier for matching the patient’s records across several
providers. Instead, clients will be matched based on automated
algorithms. Details of the procedure are provided
elsewhere.
6.
HIPAA compliant. George Mason University’s
Institutional Review Board will supervise the data safety issues related
to the proposed organization. No data will be transferred without
authentication of the provider and verification that the patient has
signed a consent form. Participating organizations will maintain the
signed consent forms of the patients.
7.
Data mining & research Health care researchers will be
allowed to have access to the data after removing patient, provider and
organization’s unique identifiers.
8.
Personal records. Patients will be allowed to review
their records and suggest changes to participating organization.
9.
Online health education. Patients will have access to
confidential health information tailored to their needs.
10.
Public health monitoring. RHIO will allow public
health agencies to use the data to monitor outbreak of diseases.
11.
CMS review organizations. RHIO will work with Center
for Medicare and Medicaid Services peer-review organizations to provide
assistance in analysis of improvement trends.
12.
Free EMR to small and safety net clinics. RHIO will
provide the Veteran Administration’s Vista Electronic Medical Record
free of charge to all participating clinical groups of less than 12
clinicians. In addition, RHIO will provide free training and
maintenance services for these clinics if the State supports the
University in accomplishing these goals.
It seems odd to think of all the changes in the rest of our lives
brought about by the internet and then to go and sit in the waiting room
of a doctors office and read old People magazines and fill out paper
forms. Ultimately healthcare will be as different as airline
reservations and banking have become, or more. We are seeing, in some
places, truly modern information enhanced practices with EHRs spring up
and thrive. The ruts of the past are deep, but the need for advanced
practices is too strong to resist. Existing practices are gradually
enhancing their appeal by adding virtual elements. So the first
competition will be avant-guard providers reaching out over the web and
taking patients away from plain waiting rooms. Patients who see value in
this and respond by putting up with the inevitable bumps in the road
will be able to shape the future of healthcare.
Lærum H, Ellingsen G, Faxvaag A.
Doctors' use of
electronic medical records systems in hospitals: cross sectional survey.
BMJ 2001;323:1344-1348 ( 8 December )
Mitchell E, Sullivan F.
A descriptive
feast but an evaluative famine: systematic review of published articles
on primary care computing during 1980-97 BMJ, Feb 2001; 322:
279 - 282.
Majeed A, Lusignan SD, Teasdale S.
Ten ways to
improve information technology in the NHS • Commentary: improve the
quality of the consultation • Commentary: Clinical focus might make it
work BMJ, Jan 2003; 326: 202 - 206.
Mandl KD, Szolovits P, Kohane IS, Markwell D, MacDonald R.
Public standards
and patients' control: how to keep electronic medical records accessible
but private • Commentary: Open approaches to electronic patient records
• Commentary: A patient's viewpoint BMJ, Feb 2001; 322: 283 - 287.
The following additional resources are available to help you think
through this lecture:
u
Prepare to present one of the articles in the reading set.
|